About axSpA
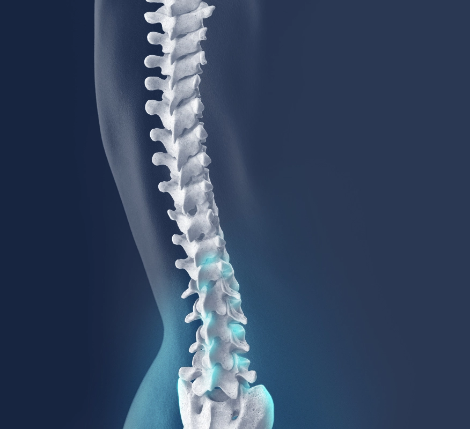
Axial spondyloarthritis (also known as axSpA or axial SpA) is one of a group of inflammatory rheumatic diseases known as spondyloarthritis that share clinical and genetic features.
AxSpA is a progressive chronic inflammatory disease that primarily affects the spine and the sacroiliac (SI) joints that connect the lower spine to the pelvis.
This results in pain and stiffness in the lower back, hips and buttocks. It can also affect other joints in the body, as well as tendons and ligaments. It causes inflammation and can lead to chronic pain, and impairments in mobility.
LEADING SYMPTOM:
Inflammatory back pain, particularly morning back stiffness, that improves with exercise but not with rest
DISEASE ONSET:
Insidious, slow onset, usually before the age of 45, often in the 20s
PREVALENCE:
Varies across the globe, but could be as many as 1 in 150 people
axSpA has two forms:
Non-radiographic axSpA (nr-axSpA)
There are symptoms and inflammation can occur. But damage to the sacroiliac joints (SIJ) is not visible on X-ray.
MRIs can help diagnose nr-axSpA.
Radiographic axSpA (r-axSpA)
sometimes known as ankylosing spondylitis (AS) or Morbus Bechterew
Damage to the spine or SIJ is visible on X-ray.
This doesn’t usually occur until a number of years after first symptoms.
Over time, AS can cause some of the vertebrae to fuse together, which makes your spine less flexible and can make it difficult to straighten the back and neck; in some severe cases this can lead to a stooped posture, known as kyphosis.
Some people diagnosed with nr-axSpA may, over time, develop damage in the SIJ comparable to r-axSpA (AS).
However, not all patients will progress or experience fusion of the spine.
Symptoms
The main symptom of axSpA is pain in the spine and sacroiliac joints, caused by chronic inflammation.
Symptoms vary from person to person, but almost always include:
- • Symptoms which start before the age of 45 (can occur in children or rarely later in life)
- • Persistent lower back pain for more than 3 months
- • Pain and stiffness, which improve with activity and exercise and worsen with rest – especially overnight and morning stiffness that lasts 30 minutes or more
- • Pain which responds well to non-steroidal anti-inflammatory drugs (for example ibuprofen).
Other symptoms can include:
- • Pain in the hips or buttocks (rarely with pain shooting down the leg)
- • Limited spinal flexibility which can become severe and affect daily life
- • Fatigue
- • Widespread pain.
Associated conditions
Sometimes, people also have associated conditions; some of the most common are:
- • uveitis, a form of eye inflammation that causes eye redness, pain and sometimes blurred vision
- • inflammatory bowel diseases (IBD), mainly Crohn’s disease and sometimes ulcerative colitis that cause chronic inflammation of the gastrointestinal (GI) tract
- • psoriasis, a skin condition that causes red, itchy, scaly patches
- • peripheral arthritis, arthritis occurring in parts of the body, other than the spine and SIJ
- • enthesitis, inflammation where ligaments and tendons connect with bones, such as heel or ribs
- • dactylitis or ‘sausage digits’, inflammation that causes the fingers or toes swell up.




Other associated conditions that may be experienced are anxiety and depression, cardiovascular disease, pulmonary and renal diseases and genitourinary conditions.
People with spinal fusion from axSpA are at an increased risk of fractures of the spine.
Why do people get axSpA?
There is still more to be learned about what causes axSpA, but we know it is an immune-mediated and inflammatory disease.
Family history and genetics can be important; there is a higher chance of developing it if a first-degree relative (for example, a parent or sibling) has it.
HLA-B27, a genetic marker is often present in axSpA patients. However, having the gene does not mean that you will develop axSpA; it simply means there may be an increased probablity of developing it.
While it was historically, and incorrectly, considered a predominantly male disease,axSpA affects men and women equally. People of all races and from all parts of the world can have the disease, but it is more common in northern parts of the world.
If you are aware of axSpA in your family and you have symptoms, it is important to mention this to your doctor. If you do have axSpA, it may speed up your diagnosis and time to appropriate treatment.
Diagnosis
Getting a diagnosis of axSpA can take some time and involve different tests and doctors. There is no single diagnostic test, which means many people who live with it can wait years for a diagnosis.
Non-radiographic axSpA can be especially difficult to diagnose, because the skeletal damage cannot be seen on an X-ray.
If there is a suspicion a person has axSpA, they should be referred to a specialist; it should be a rheumatologist who investigates and makes a diagnosis.
Diagnosis of axSpA does vary around the world and from one healthcare system to another, but typically a diagnosis will be made with some, or all, of the following steps:
- • Medical history is reviewed, particularly focussing on when and how symptoms started
- • The inflammation will be assessed to see how it is affecting the entire body, including looking for other associated conditions (see ‘symptoms’ above)
- • Physical examinations help determine the level of pain and tenderness, as well as mobility and stiffness
- • Blood tests are carried out to identify the HLA-B27 gene
- • Blood tests can also be used to detect inflammatory markers (an increase in certain proteins, which are sometimes present with inflammation)
- • X-rays show if there is damage to the bones or joints – often the spine or sacroiliac joints - including if extra bone has grown or fusion has occurred
- • MRI can show if there is inflammation around your joints in the soft tissue; this cannot be detected by an X-ray and so MRI is often needed to diagnose nr-axSpA.
Managing axSpA
Doctors are likely to prescribe a combination of regular exercise and medication to help manage the pain.
Physical therapy and exercise are the most important things you can do to alleviate axSpA symptoms and maintain wellbeing. The fitter and more flexible you are, the better you will be able to deal with symptoms. A doctor will likely recommend specific exercises that promote spinal extension and mobility in order to maintain posture, range of motion and mobility, to help alleviate pain, and to prevent the bones and joints from getting ‘locked’ into place and to minimise deformities.
Medication can reduce inflammation, help with the pain and enable you to continue exercising.
Joint damage cannot be reversed, but medications can help slow further damage. Your doctor may recommend one or a combination of the following therapies to manage the inflammatory pain and slow disease progression:
• Nonsteroidal anti-inflammatory drugs (NSAIDs) – these reduce inflammation and associated pain; ibuprofen is a commonly used NSAID. NSAIDs are often a first treatment option because they are so effective
• Corticosteroid – these are steroids, used to control inflammation, usually in the form of an injection
• Biologic drugs and biosimilars – these work by inhibiting the body’s production of inflammation
• Disease-modifying anti-rheumatic drugs (DMARDs) – these are commonly used to help if you have pain and stiffness in peripheral parts of the body, such as ankles or wrists - but are not shown to be effective for back pain.

Treatment options
Living well with axSpA
Check if your symptoms could indicate axSpA
Symptom checkers

BULGARIAN

Are you a healthcare professional?
Watch Dr Raj Sengupta, an expert rheumatologist, outline the way axSpA presents clinically as well as the importance of achieving a timely diagnosis. Patients share their experiences to clearly illustrate Dr Sengupta’s points.
